radiation
there are many different types of radiation used to treat various types of benign and malignant tumors. the "standard" or "original" type of radiation is photon-based radiation. nowadays, there's also proton-based radiation and stereotactic radiosurgery (SRS). the main difference between photon- and proton-based radiation is that photon beams target the tumor and pass through the other side, whereas proton beams stop at the target. despite the name, SRS isn't surgery; it's a highly-targeted high-dose treatment.
(there's also carbon ion therapy, brachytherapy, and others that aren't as relevant for meningiomas.)
for meningiomas, a few types of radiation are most commonly used1:
- photon-based radiation (EBRT, IMRT, VMAT)
- proton beam therapy
- stereotactic radiosurgery (gamma knife, cyberknife or other LINAC-based SRS, SRT/FSRT)
here's a comparison chart highlighting some of the pros and cons to each type:
| Feature | Photon-based IMRT | Proton therapy | SRS (Gamma Knife, Cyberknife, LINAC) |
|---|---|---|---|
| Precision | High (dose sculpting possible, but some spillover beyond target) | Very high (Bragg peak stops protons at tumor depth, minimal exit dose) | Extremely high (sub-millimeter targeting, steep dose fall-off) |
| Typical Schedule | Daily treatments, 5 days/week, for 5–6 weeks | Daily treatments, 5 days/week, for 5–6 weeks | Usually 1 session (single-fraction SRS), or 3–5 sessions (fractionated SRS) |
| Tumor Size Suitability | Medium–large tumors | Medium–large tumors, esp. near sensitive structures | Small–medium tumors (<3–4 cm) with well-defined borders |
| Best For | Tumors close to optic nerve/brainstem; atypical or malignant meningiomas needing wide coverage | Tumors near critical structures (optic apparatus, pituitary, brainstem); younger patients (to reduce long-term risk) | Small, benign meningiomas in accessible locations, often in skull base or convexity |
| Advantages | Widely available; proven; flexible for irregular shapes | Lower radiation to healthy brain; reduced long-term toxicity; more favorable for younger patients | Non-invasive; highly precise; usually single outpatient treatment; lower cumulative radiation to brain |
| Limitations | Higher radiation exposure to surrounding brain than protons | Limited availability; expensive; longer treatment course | Not ideal for large tumors or when tumor touches critical structures (risk of radiation injury if single high dose used) |
the most common type of radiation treatment i've read about skull base meningioma patients undergoing is SRS. within SRS, gamma knife seems to be the more preferred option as it offers over 100 initiation points of radiation vs LINAC machines, which offer only one initiation point. however, SRS is not always available to patients due to the size of their tumor, where they're located, and other factors.
gamma knife radiosurgery can be administered in one single dose or in 3-5 fractionated doses. single session SRS is best for small, benign, well-defined meningiomas that are not hugging critical structures, whereas fractionated SRS is preferred when the tumor is close to essential structures, such as the brainstem or cranial nerves.
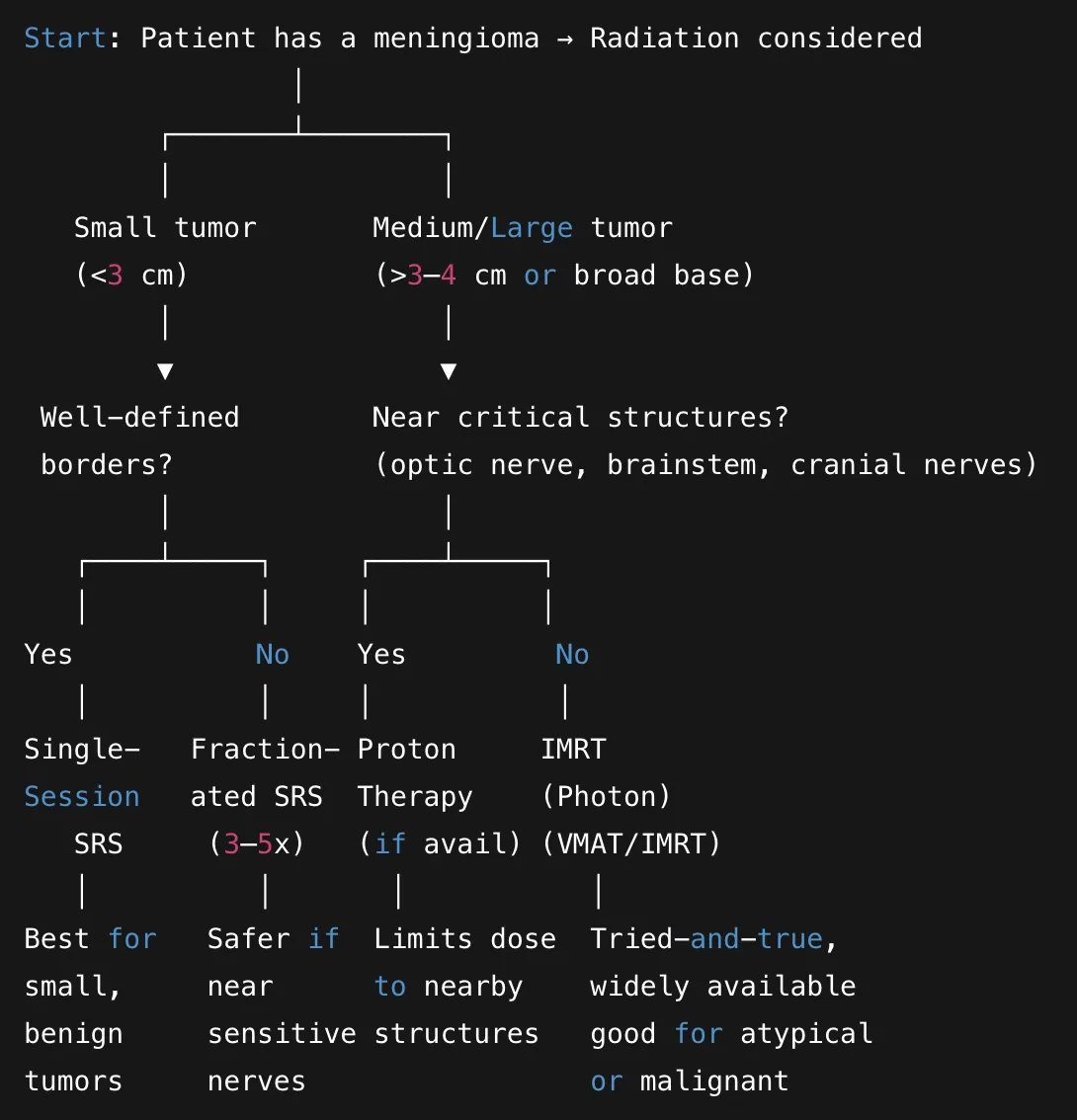
here's a very simplified decision tree a radiation oncologist might follow to determine which type of radiation is best for a particular patient:
hopefully this provides you with a better basic understanding of the various types of radiation used to treat meningiomas so that you have a more solid starting point in your conversation with your radiation oncologist.
--
additional reading & resources:
- stereotactic radiation treatment for benign meningiomas
- 2025 journal article on where radiation oncologists stand on radiation for meningiomas today
- 2016 study reviewing photon and proton therapy for skull base tumors
- 2011 study on the long term effect of FSRT on skull base benign meningiomas
--
footnotes: